Chronic Fatigue Syndrome (CFS) is a multi-factorial condition that requires a holistic and thorough approach to treatment. I did my MSc dissertation on cortisol resistance in chronic fatigue syndrome so I have spent considerable amounts of time in the research.
What Are The Symptoms Of Chronic Fatigue Syndrome?
Typical symptoms include post-exertional fatigue, memory or concentration problems, muscle pain, joint pain, headaches, sore throat, painful swollen lymph nodes and sleep disturbance. Digestive symptoms such as bloating and bowel irregularities are also common.
A statistic from a ‘2020 Health’ report stated that:
The total cost to the UK economy of CFS in 2014/15 was at least £3.3 billion
In this article I want to cover some of the underlying causes of this condition.
I also recently recorded this webinar which goes through the numerous underlying causes of chronic fatigue:
Can Gut Issues Cause Chronic Fatigue Syndrome?
In analogy with “the atopic march” in allergic diseases, we suggest “a dysbiotic march” in IBS; initiated by extensive use of antibiotics during childhood, often before school age. Various abdominal complaints including IBS may develop soon thereafter, while systemic symptom like CFS and fibromyalgia may appear years later.
Dysbiosis (imbalances in our gut bacteria) have been associated with CFS. This may contribute to low grade inflammation which has been associated with CFS. Previous causes of antibiotics, other medications such as PPI’s, a poor diet (high in sugar in low in vegetables and phytonutrients), chronic stress can call contribute to imbalances in our gut bacteria.
Research has also found lower microbiome diversity in patients with CFS.
Leaky Gut And Chronic Fatigue
Leaky gut has been associated with CFS. Leaky gut is a condition when the lining of our digestive system becomes excessively permeable allowing bacterial remnants and undigested food particles into our circulation where they can trigger a chronic immune response and low level inflammation.
Click here for a research paper discussing this connection.
SIBO And Chronic Fatigue
SIBO can cause inflammation, leaky gut and nutrient deficiencies which may all contribute to a CFS. One paper did find that:
77% of participants with CFS had SIBO.
SIBO stands for ‘small intestine bacterial overgrowth’.
Click here for my blog post introducing SIBO, and click here, for a study demonstrating this link.
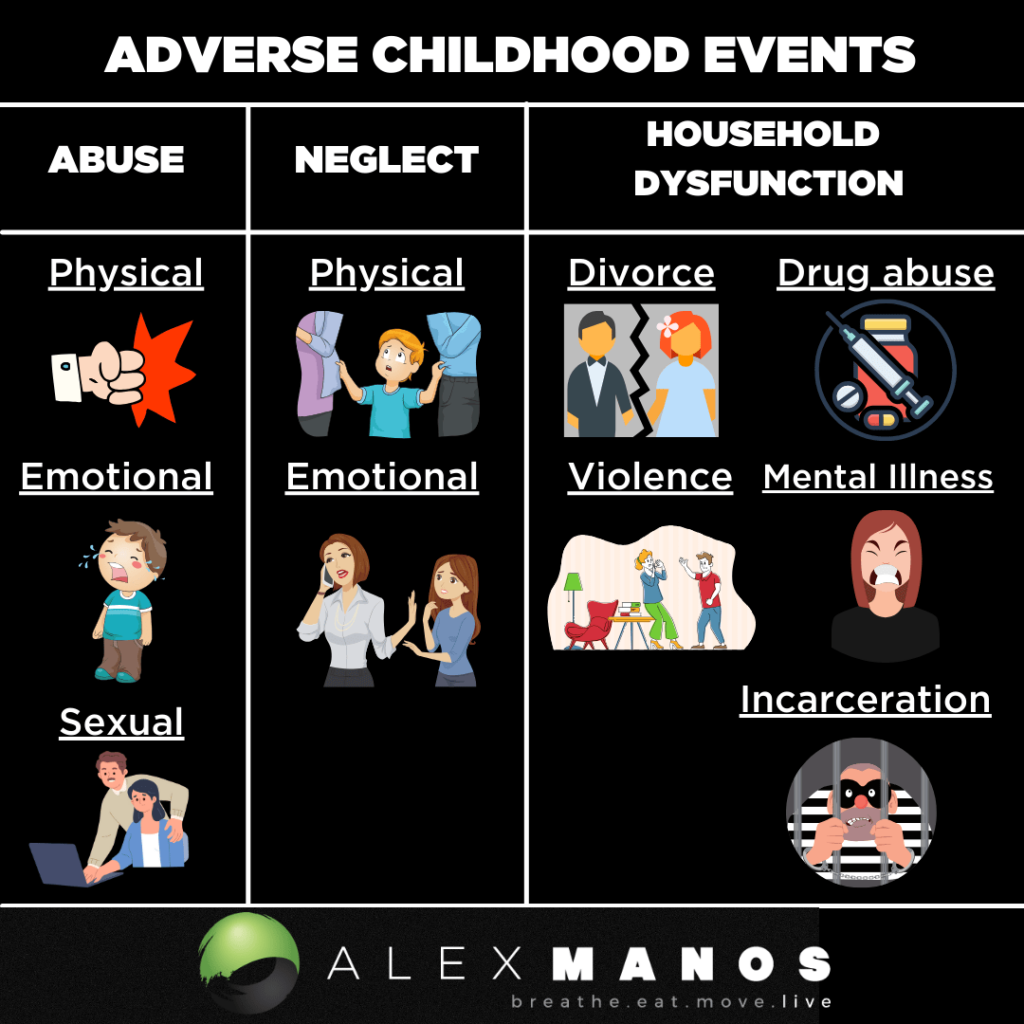
Adverse Childhood Events
A growing literature suggests that early adverse experience increases the risk for a range of negative health outcomes, including fatiguing illnesses. (source)
In a case-control study of 43 cases with current CFS and 60 non-fatigued controls the authors concluded that their results suggested that childhood trauma is an important risk factor for CFS.
Mitochondrial Dysfunction Causes Chronic Fatigue Syndrome
Using a test that measures the availability of ATP and the efficiency of oxidative phosphorylation in mitochondria, it was found that all tested individuals with CFS/ME had evidence of mitochondrial dysfunction, as compared to controls, and this dysfunction was cor- related with the severity of the illness. This finding is supported by other studies indicating the involvement of mitochondrial dysfunction.
Evidence of CoQ10 deficiency in CFS/ME provides further support for mitochondrial involvement, as CoQ10 status has been proposed as a measure of mitochondrial function.CoQ10 deficiency has been shown to decrease expression of proteins involved in mitochondrial energy metabolism, reduce mitochondrial membrane potential, increase production of reactive oxygen species, and result in the degradation of dysfunctional CoQ10-deficient mitochondria.
You may find this book, click here, helpful.
Can A Viral Infection Cause Chronic Fatigue Syndrome?
Viral infections have been associated with CFS.
In conclusion, this study using both serological and PCR-based techniques for distinguishing between active and latent infection showed high rate of active EBV infection among patients with ME/CFS indicating that at least in a subset of cases, EBV is important factor for the development of disease.
The most frequently discussed virus to be associated with CFS is the Epstein-Barr Virus. A great book on this topic is The Epstein Barr Virus Solution by Dr. Kines: click here.
Other viruses discussed in the research include the Ross River virus, enterovirus, harper complex viruses (HHV-6A & 6B) and Parvovirus B19.
Can Mycotoxins Cause Chronic Fatigue Syndrome?
Mycotoxins can contribute to CFS and this has also been discussed in the research.
Environmental Toxins
A number of reports have linked toxins—including pesticides and insecticides, mercury, lead, and nickel —to CFS/ME or chronic, fatigue-like symptoms.
Cadmium and tobacco smoke have also been hypothesised to play a role.
Because these reports are limited by several factors, such as variable exposure and outcome measurements, small sample sizes, and unreliable CFS/ME definitions, they provide only weak evidence of an association; however, further research in this area appears warranted.
In an illustrative study, serum organophosphates in CFS/ME participants were found to be higher than in control participants and comparable CFS/ME participants with a known chemical exposure.This finding suggests a possible role for low-level bioaccumulation of persistent organic pollutants in the development of CFS/ME.
Inflammation And Oxidative Stress
Inflammation and oxidative stress have been proposed as fundamental pathological features of CFS/ME, and several independent investigations have found evidence of distinct elevations in chronic, low-grade inflammation and oxidative stress in CFS/ME sufferers compared to healthy controls.
For example, one study found significantly increased levels of C-reactive protein (CRP) in participants with CFS/ME versus healthy participants. In another investigation, peroxide concentrations were significantly higher in participants with CFS/ME and distinctly differentiated participants with CFS/ME from healthy controls.
And some evidence suggests that elevations in oxidative stress correlate directly with symptom severity.
Is Chronic Fatigue Syndrome An Autoimmune Condition?
ME/CFS disease onset is often reported to be triggered by infections and the link between infections and autoimmune diseases is well established. Although the exact pathogenesis is still unknown, the most plausible hypothesis is that dysregulation of immune system, autonomic nervous system and metabolic disturbances contribute to this complex syndrome, in which severe fatigue and cognitive impairment are a central feature. Stressful life events are frequently associated with disease onset concomitantly with a history of frequent recurrent infections, immune deficiency and autoimmunity. There are numerous studies showing immunological, genetic and metabolic alterations consistent with an autoimmune mechanism.
Further, the identification of autoantibodies in ME/CFS patients and the clinical benefit associated with B cell depleting therapy provide strong evidence that, at least in a subset of ME/CFS patients, the disease has an autoimmune etiology.
CFS, Infections And Autoimmune Disease
Infection by various pathogens, including the Epstein-Barr virus (EBV), the human herpes virus (HHV)-6 and the human parvovirus B19, but also intracellular bacteria, are known as triggers of disease. In a subset of patients, ME/CFS begins with infectious mononucleosis and evidence for a potential role of EBV in ME/CFS comes from many studies. In 1984, DuBois et al. first described patients with mononucleosis syndrome suffering from long-lasting fatigue and serological evidence of EBV reactivation followed by a number of studies describing ME/CFS patients with serological evidence of chronic active EBV infection.
Infectious mononucleosis is known as a risk factor for various autoimmune diseases.
Several studies show homologies of EBV sequences with human autoantigens such as myelin basic protein for multiple sclerosis (MS)
Autoantibodies And Chronic Fatigue Syndrome
Autoantibodies are antibodies (a type of protein), produced by the immune system, that is directed against one or more of our own proteins. Many autoimmune diseases (notably Lupus) are caused by such autoantibodies.
Several studies described autoantibodies in ME/CFS
Antinuclear antibodies (ANA) were found in one study in 68 % of ME/CFS patients.
Antibodies against:
- The muscarinic M1 acetylcholine receptor (AChR)
- ß1 and ß2 adrenergic receptors (AdR)
- Thyroid peroxidase autoantibodies
- Serotonin
Inflammation, Autoimmune Disease, And Chronic Fatigue Syndrome
Autoimmunity is associated with enhanced levels of circulating inflammatory molecules playing an important role in the pathogenesis of autoimmune diseases.
Elevated levels of cytokines (inflammatory molecules) have been reported for CFS in several studies.
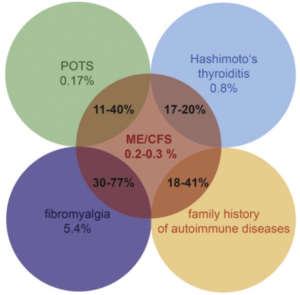
Comorbidity with autoimmune diseases
Comorbidity of CFS with various autoimmune or immune-mediated diseases including fibromyalgia (FM), Hashimoto’s thyroiditis and POTS is observed. Especially for FM there is considerable overlap with up to 77% of patients fulfilling disease criteria for both CFS and FM. FM is characterized by chronic widespread pain and is common in autoimmune diseases with around 50% of prevalence in patients with Rheumatoid Arthritis and Lupus.
 Summary
Summary
- The pathogenesis of ME/CFS is multifactorial, and immunological and environmental factors play a role.
- Autoimmune mechanisms can be linked with ME/CFS at least in a subset of patients.
- Autoantibodies mostly against nuclear and neurotransmitter receptors are found in a subset of ME/CFS patients.
- Immunomodulatory therapeutic strategies targeting autoantibodies may be beneficial and should be pursued.
Treatment Considerations
It is important to appreciate we must “treat the individual, not the disease”, as the saying goes. You may like to read by blog on Narrative Medicine to learn about the importance of honouring the story of the patient when it comes to healing and the therapeutic relationship.
As a result I think it is really important interventions are based on a sound understanding of your symptoms, health and medical history and your life story/journey. Things we need to consider include:
- Gut health: How many courses of antibiotics have you taken? Has your diet been supporting a healthy and diverse microbiome? Have you taken other medications that might negatively impact the gut?
- Stress: Did you experience any adverse childhood events? Have you experienced acute or chronic stress in adolescence or adulthood?
- Environmental toxins: Have you lived/worked/stayed in a property that had water damage, such as a water leak? Have you lived in a property with visible damp issues, or mould? Do you have amalgam fillings? Do you, or did you smoke? Have you had a profession that might expose you to various chemicals?
- Nutrient Status: Could an iron deficiency been contributing to your fatigue? Are you vegan/pescatarian/vegetarian? Do you have low stomach acid or have an H. Pylori infection? If we evaluate your diet, and past eating behaviour, do we suspect you may have developed some nutrient deficiencies that could contribute to fatigue in some way – poor mitochondrial health or immune health for example?
- Immunity: Did you have glandular fever when you were younger? If so, then you may reactivated Epstein Barr virus. Or were there any other signs of an acute infection? When travelling for example?
If you’ve tried dietary changes, if your’ve tried supplements and other types of therapies then you may like to check out the Gupta Program also. For some this is the missing piece in their puzzle.
Learn more about the program by listening to my interview with the founder, Ashok.
References
- Is SIBO A Real Condition? Click here.
- Rasa et al., (2018) Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome, J Transl Med 16:268 (click here)
- Proal A and Marshall T (2018) Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in the Era of the Human Microbiome: Persistent Pathogens Drive Chronic Symptoms by Interfering With Host Metabolism, Gene Expression, and Immunity. Front. Pediatr. 6:373 (click here)
- Sepúlveda N, Carneiro J, Lacerda E and Nacul L (2019) Myalgic Encephalomyelitis/Chronic Fatigue Syndrome as a Hyper-Regulated Immune System Driven by an Interplay Between Regulatory T Cells and Chronic Human Herpesvirus Infections. Front. Immunol. 10:2684 (click here)
- Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria (click here)
- Inflammatory and oxidative and nitrosative stress pathways underpinning chronic fatigue, somatization and psychosomatic symptoms (click here)
- Gut Microbiota, Bacterial Translocation, and Interactions with Diet: Pathophysiological Links between Major Depressive Disorder and Non-Communicable Medical Comorbidities (click here)
- Myalgic Encephalomyelitis/CFS in the Era of the Human Microbiome: Persistent Pathogens Drive Chronic Symptoms by Interfering With Host Metabolism, Gene Expression, and Immunity (click here)
- Cytomegalovirus, Epstein-Barr virus, and human herpesvirus-6 infections in patients with myalgic еncephalomyelitis/chronic fatigue syndrome (click here)
- From IBS to ME – The dysbiotic march hypothesis (click here)
- Metabolic Dysfunction in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Not Due to Anti-mitochondrial Antibodies (click here)


 Summary
Summary
