With magnesium often claimed to be one of the most common nutrient deficiencies, and with so many clients asking about the nutrient I thought I would start creating a ‘master document’ on this amazing nutrient.
What Is Magnesium?
Magnesium is the second most abundant intracellular cation, after potassium, and is the fourth most abundant cation in the human body (cation meaning it is negatively charged). This essential mineral is needed for a broad variety of physiological and biochemical functions. As a co-factor in more than 300 enzymatic reactions, which often depend on ATP (energy), magnesium is involved in many biochemical pathways of key importance, including:
- The degradation of macronutrients (such as fats from our diet)
- Oxidative phosphorylation (energy production)
- DNA and protein synthesis
- Neuro-muscular excitability
- Regulation of parathyroid hormone secretion
As a physiological calcium channel antagonist, magnesium affects processes that are regulated by intracellular calcium concentration fluxes and is therefore essential for normal neurological and muscular function.
Furthermore, magnesium regulates cell membrane permeability via interactions with phospholipids and affects vessel tone and blood pressure.
More than 99% of the total body magnesium is located in the intracellular space, mainly stored in bone (60-65%), muscle and soft tissues (34-39%), whereas less than 1% is located in the extracellular space. This makes testing for magnesium status very hard (more on this later!).
Best Food Sources Of Magnesium
Dark leafy greens (e.g kale, spinach), oatmeal, buckwheat, whole grains, chocolate, nuts & seeds, lima beans and molasses, fish, meat, dairy foods.
Magnesium Deficiency
There are two types of nutrient deficiencies:
- Frank deficiencies (such as scurvy from ascorbic acid deficiency or goitre from iodine deficiency).
- Subclinical deficiencies (a clinically silent reduction in physiological, cellular and/or biochemical functions).
It is the latter that is most concerning as it is hard to diagnose and predisposes to numerous chronic diseases. And while both result in negative health consequences, the former has obvious symptoms (hence frank deficiency), whereas the latter may have negative or variable health effects that are not so apparent (eg. vascular calcification).
The evidence in the literature suggests that subclinical mg deficiency is rampant and one of the leading causes of chronic diseases including cardiovascular disease and early mortality around the globe, and should be considered a public health crisis (1)
The Symptoms Of Magnesium Deficiency
Cardiac arrhythmia, palpitations, weakness and fatigue, ataxia (loss of full control over body movements), muscle twitches and spasms, low blood levels of calcium and related disorders such as tetany and osteomalacia, low blood levels of potassium, apparent vitamin D deficiency and resistance to standard treatment.
More moderate magnesium deficits may contribute to the following disorders: osteopenia and osteoporosis, soft tissue calcification (such as kidney stones), high blood pressure (hypertension), preeclampsia and eclampsia, migraines, and many aspects of cardiovascular disease.
Recommend Intake
Balance studies suggest a daily Mg2+ requirement of 3.0- 4.5 mg per kg body weight.
Whereas the Institute of Medicine recommends 310-320 mg per day for women and 400-420 mg per day for men as adequate, the European Food Safety Authority recently defined an adequate intake of 300 and 350 mg per day for women and men, respectively.
Absorption
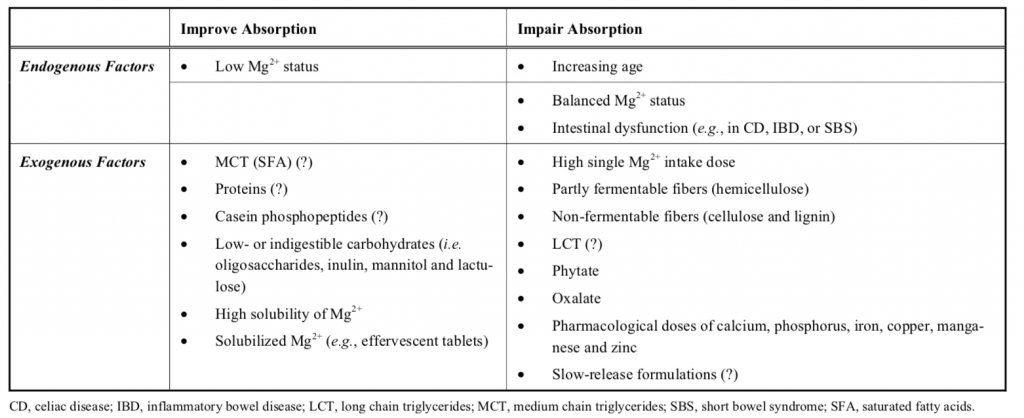
Various factors influence the intestinal uptake of magnesium and are of substantial importance for the supply of the mineral. Dietary magnesium uptake in the intestine varies within a broad range and depends on dose, the food matrix, and enhancing and inhibiting factors. Furthermore, several studies have shown that the absorption of magnesium from food supplements and pharmaceutical preparations under standard conditions is slightly influenced by the type of magnesium salt. Nevertheless, an approach that focuses on one or a few aspects is insufficient from a nutritional and medical point of view.
To understand the true absorption of magnesium, numerous endogenous and exogenous factors must be considered. Overall, the understanding of magnesium absorption and its influencing factors is still limited, which has been due to methodological limitations.
Intestinal magnesium absorption occurs pre-dominantly in the small intestine via a paracellular pathway, and smaller amounts are absorbed in the colon, mainly via a transcellular pathway. In humans, magnesium absorption starts approximately 1 h after oral intake, reaches a plateau after 2-2.5 h up to 4-5 h and then declines. At 6 h, the magnesium absorption is approximately 80% complete.
With a daily intake of 370 Mg, the absorption rate of magnesium in the intestine ranges from 30-50%. However, the efficiency of magnesium uptake is dependent on the ingested dose. For example, early studies with a low dietary magnesium intake showed that the relative absorption rate can reach 80%, whereas it is reduced to 20% with magnesium surfeits.
(Schuchardt & Hahn, 2017)
Absorption of magnesium from different kinds of magnesium supplements varies. Forms of magnesium that dissolve well in liquid are more completely absorbed in the gut than less soluble forms.
Small studies have found that magnesium in the aspartate, citrate, lactate, and chloride forms is absorbed more completely and is more bioavailable than magnesium oxide and magnesium sulfate. (source)
One study found that very high doses of zinc from supplements (142 mg/day) can interfere with magnesium absorption and disrupt the magnesium balance in the body
What Causes Magnesium Deficiency?
Numerous factors can lead to deficiency, including:
- Kidney failure.
- Alcohol consumption.
- Malabsorption issues (magnesium is absorbed in the small intestine and in the colon; thus, patients with intestinal or colon damage such as Crohn’s disease, irritable bowel syndrome, coeliac disease, gastroenteritis, ulcerative colitis, may have magnesium deficiency).
- Supplementing with calcium can lead to magnesium deficiency due to competitive inhibition for absorption.
- Over supplementing with vitamin D may lead to mg deficiency via excessive calcium absorption.
A meta-analysis of 13 studies in almost 5500 patients found that mg levels were significantly lower in patients with metabolic syndrome versus controls. (1)
Cardiovascular Health
We concluded that high Mg intake is associated with lower risk of major CV risk factors (mainly metabolic syndrome, diabetes and hypertension), stroke and total CVD. Higher levels of circulating Mg are associated with lower risk of CVD, mainly ischemic heart disease and coronary heart disease (Rosique-Esteban et al., 2018).
The Gut Microbiome
Animal studies suggest that magnesium deficiency can contribute to a decline in bacterial diversity.
Testing Magnesium Status
- Serum magnesium
- Red blood cell magnesium (LabCorp, Quest)
- 24-Hour urine magnesium (LabCorp, Q uest)
Serum magnesium declines in deficiency and rises in toxicity, but it is less sensitive than red blood cell and urine to changes in magnesium status. Red blood cell magnesium may be low when serum is not, and while this could indicate an early deficiency, it could also indicate a deficiency in factors needed for bringing Mg into cells, such insulin signalling, energy production, and sodium. Urine magnesium will be low in nutritional deficiency, but high in deficiencies caused by urinary loss.

The interpretation of Mg markers is best facilitated by taking all three measurements. A nutritional Mg deficiency is likely to produce low values across all three measurements. Low blood values coupled to high urine values reveal urinary Mg wasting. A large discrepancy between serum and red blood cell magnesium could suggest a problem with magnesium transport.
Most Reliable Test
Thoren’s intravenous mg load test (16 hours)
Retention of magnesium load (intravenous or oral) after its administration is likely the best indicator of mg deficiency. However, the retention test assumes normal kidney function for intravenous mg loads and normal gastrointestinal and renal function for oral load tests and is cumbersome and invasive.
Unreliable Ways To Test For A Magnesium Deficiency
- Hair mg content (one study concluded: ‘mg hair concentration may be an easier, cheaper and less invasive indicator of body Mg depletion’).
- Bone mg (mg depletion in the coccyx may indicate Mg deficiency).
- Ratio of ionised magnesium to total mg (serum or plasma).
- Lymphocyte magnesium.
- Urinary or faecal mg excretion (low or high levels may indicate deficiency).
- Urinary fractional mg excretion >4% (some authors have suggested >2% in those with normal kidney function).
- Total erythrocyte mg levels.
- Total serum mg levels.
Supplementing Magnesium
Absorption of magnesium from different kinds of magnesium supplements varies. Forms of magnesium that dissolve well in liquid are more completely absorbed in the gut than less soluble forms . Small studies have found that magnesium in the aspartate, citrate, lactate, and chloride forms is absorbed more completely and is more bioavailable than magnesium oxide and magnesium sulfate [12-16]. One study found that very high doses of zinc from supplements (142 mg/day) can interfere with magnesium absorption and disrupt the magnesium balance in the body
How Much Magnesium Should I Supplement?
One group of authors concluded: ‘When mg substitution is started, the minimum dose to be applied is 600 mg mg per day.The therapy should proceed for more than one month, and then continue with a dose that holds the serum value not lower than 0.9mmol/L mg’. The authors noted that using a cut-off of 0.75mmol/L for mg deficiency misses 50% of those with true mg deficiency. (1)
References
Di Nicolantonio JJ, O’Keefe JH, Wilson W. Subclinical mg deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart 2018
Jan Philipp Schuchardt & Andreas Hahn (2017) Intestinal Absorption and Factors Influencing Bioavailability of mg – An Update, Current Nutrition & Food Science, 13, 260-278 click here
Rosique-Esteban et al., (2018) Dietary Mg and Cardiovascular Disease: A Review with Emphasis in Epidemiological Studies, Nutrients. 2018 Feb 1;10(2) click here
Winther G et al (2015) Dietary mg deficiency alters gut microbiota and leads to depressive-like behaviour, Acta Neuropsychiatr. Jun;27(3):168-76 click here